By Dr. Petrus Raulino
The more research advances, the more we see that aspects of mental life, such as anxiety, concentration and memory, are intertwined on complex and dynamic biological bases.
Understanding that there are biological bases that influence alterations in mental life is also a way of combating stigmas and mistaken myths. We make fewer mistakes when we understand that mind and brain are interconnected and don't work separately.
According to a publication by Agência Fapesp, a study carried out at UNICAMP suggested that COVID-19 can alter the brain's connectivity pattern even in cases of mild COVID-19.
The data, which is still preliminary, seems to indicate that COVID-19 can cause a kind of "short circuit" in the organ.
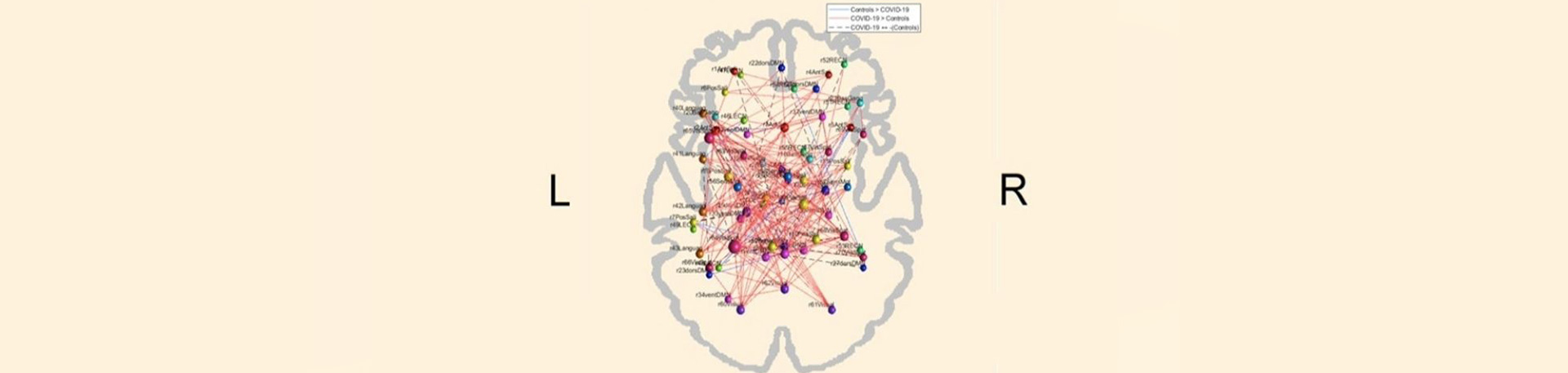
In the study, 86 volunteers with COVID-19 that had been resolved for at least two months underwent functional magnetic resonance imaging scans to compare with 125 individuals who did not have the disease.
The group that had COVID-19 showed an intense loss of specificity in brain networks. This is thought to make the brain use more energy and work less efficiently.
The changes in the functional magnetic resonance imaging coincided with a series of persistent symptoms. About two months after diagnosis the individuals reported symptoms such as fatigue / tiredness (53.5%), headache (40.3%) and memory impairment (37%).
Six months after diagnosis, individuals still reported late symptoms, including fatigue / tiredness (59.5%), daytime sleepiness (36.3%), memory changes (54.2%), difficulty concentrating (47%) and anxiety symptoms (41.9%, well above the average for the Brazilian population of around 10%).
Neuroimaging tests showed that some regions of the cerebral cortex were thinner than expected, including areas related to anxiety. Other regions showed an increase in volume, probably due to edema caused by COVID-19.
So far it is not known how the virus affects the brain. It could be through direct damage by infecting brain cells or indirect damage through neuroinflammation. In either case, there may be persistent neuropsychiatric changes even after mild COVID-19.
On the one hand, the findings are surprising. On the other hand, there is already the hypothesis and some evidence that other RNA viruses can also affect the brain and cause neuroinflammation.
The dengue virus is an example. Research shows that around 60% of dengue patients have significant levels of anxiety and depression. And 25% of dengue patients persist with depression even after the dengue has resolved. There is also research into the long-term action of the dengue virus on the human brain.
What hypothesis could serve as a biological link between dengue fever and depression, or even COVID-19 and depression? Based on recent research, neuroinflammation is an excellent hypothesis.
BIBLIOGRAPHICAL REFERENCES:
Hashmi, A. M., Butt, Z., Idrees, Z., Niazi, M., Yousaf, Z., Haider, S. F., & Bhatti, M. R. (2012). Anxiety and depression symptoms in patients with dengue fever and their correlation with symptom severity. The International Journal of Psychiatry in Medicine, 44(3), 199-210.
Lagos-Gallego, M., Cardona-Ospina, J. A., Gutiérrez-Segura, J. C., Lagos-Grisales, G. J., & Rodriguez-Morales, A. J. (2018). Depression as acute and chronic manifestation of dengue and chikungunya: A systematic review and meta-analysis. International Journal of Infectious Diseases, 73, 373.
Klein, R. S., Garber, C., Funk, K. E., Salimi, H., Soung, A., Kanmogne, M., ... & Cain, M. (2019). Neuroinflammation during RNA viral infections. Annual review of immunology, 37, 73-95.
Johnson, T. P., Larman, H. B., Lee, M. H., Whitehead, S. S., Kowalak, J., Toro, C., ... & Nath, A. (2019). Chronic dengue virus panencephalitis in a patient with progressive dementia with extrapyramidal features. Annals of neurology, 86(5), 695-703.