Understanding dementia in Alzheimer's disease is fundamental to dealing with this complex neurodegenerative disease that affects millions of people globally.
This condition leads to the progressive deterioration of cognitive functions, such as memory and language, due to the accumulation of beta-amyloid protein plaques and the formation of neurofibrillary tangles of tau protein in the brain.
Early diagnosis is important for starting treatments that can improve patients' quality of life.
Current research focuses on new drugs, advances in imaging technologies and non-pharmacological care strategies.
Understanding these aspects not only helps in the management of the disease, but also offers hope through more effective and personalized therapies.
History of Alzheimer's dementia
The history of Alzheimer's dementia dates back to the beginning of the 20th century, when the German doctor Alois Alzheimer first described the condition in a 51-year-old patient. He observed dementia clinically characterized by profound progressive changes in the behaviour and memory of the patient, who died in 1906. On examining her brain post-mortem, Dr. Alzheimer identified a brain with a disease with distinct characteristics, such as abnormal plaques and tangles.
Since then, researchers have continued to investigate and better understand the disease. In subsequent years, additional studies have expanded knowledge about the neuropathological mechanisms that lead to Alzheimer's dementia, including the role of beta-amyloid and tau proteins in neuronal degeneration.
The discovery of genes associated with dementia in Alzheimer's disease in the 1990s and 2000s brought new information about genetic factors predisposing to the disease. These advances enabled the development of genetic tests and paved the way for more targeted studies into prevention and treatment.
Today, the history of knowledge about dementia in Alzheimer's disease continues to evolve with significant advances in neuroimaging, biomarkers and experimental therapies.
Increasing understanding of the complexity of the disease is driving the search for more effective interventions and preventive strategies to tackle this growing global public health challenge.
What is dementia in Alzheimer's disease and its medical importance?
Dementia in Alzheimer's disease - commonly called Alzheimer's dementia - is a neurodegenerative disease that mainly affects elderlyThis is characterized by a loss of functional capacity due to a progressive decline in cognitive functions such as memory and language.
Alzheimer's disease, in turn, is a set of biological changes in brain tissue characterized by the abnormal accumulation of beta-amyloid protein plaques and the formation of neurofibrillary tangles in the brain, resulting in the gradual loss of nerve cells that progressively leads to dementia.
The medical importance of Alzheimer's dementia is extremely significant due to its growing global prevalence, representing a substantial challenge for patients, caregivers and health systems.
Diagnosing the disease early is crucial to initiating appropriate therapeutic and supportive interventions, which not only help to slow down the progression of the disease, but also significantly improve the quality of life of those affected.
Currently, research is intensely focused on developing more effective treatments and preventive strategies to tackle this growing public health problem.
Continued understanding of the mechanisms underlying Alzheimer's dementia is essential to advance early diagnosis and management of the disease, offering hope for the future in the fight against this disabling condition.
Significant investments in research are being made to identify early biomarkers, explore new pharmacological and non-pharmacological therapies, and investigate genetic and environmental factors that may influence the development of the disease.
These efforts are essential to finding effective solutions that can make a tangible difference to the lives of patients and their families.
About Alzheimer's dementia
Alzheimer's dementia is a progressive and irreversible brain condition that affects more than 6.5 million Americans aged 65 and over. This condition gradually compromises memory, thinking skills and, progressively, the ability to perform simple tasks, making it the most common form of dementia among the elderly and a significant public health concern.
Although the specific causes of Alzheimer's disease are not fully known, science currently considers that the disease is essentially due to the accumulation of beta-amyloid plaques and, consequently, the formation of neurofibrillary tangles of tau protein in the brain.
These changes result in the loss of neurons and their connections, severely impacting the ability to remember, think and communicate. As it progresses, the symptoms intensify, leading to the need for complete assistance.
Initially, Alzheimer's disease manifests itself with loss of recent memory, difficulty finding words and temporal disorientation. As it progresses, mental disorganization, changes in mood and behaviour, as well as difficulties with language and coordination appear. Eventually, patients lose the ability to carry out everyday activities and recognize loved ones.
In addition to the devastating impact on patients, Alzheimer's dementia imposes a significant burden on caregivers and healthcare systems, driving up costs and requiring specialized care as the disease progresses. Continued research is crucial to improving understanding of the disease and developing more effective treatments and preventative strategies.
Education and awareness of Alzheimer's disease are essential for early diagnosis and appropriate management, promoting a better quality of life for all those affected.
Epidemiology of Alzheimer's dementia
The epidemiology of Alzheimer's dementia is proving to be a growing concern as the global population ages. It is estimated that more than 50 million people worldwide are living with Alzheimer's dementia or another form of dementia, and this number is expected to almost triple by 2050. The prevalence of dementia varies significantly by region and is closely linked to increased life expectancy.
In the United States, for example, around 6 million people have Alzheimer's dementia, and this number continues to rise. In Europe, the disease affects approximately 10 million individuals, while in Asia prevalence is also on the rise due to population aging and lifestyle changes.
The incidence of Alzheimer's dementia is higher in the elderly, with age being the main risk factor. However, cases diagnosed in younger people, although rarer, indicate a variety in the presentation of the disease.
The growing social and economic burden of Alzheimer's dementia increases the urgent need for public health policies that support early diagnosis, integrated care and ongoing research into more effective treatments.
This epidemiological understanding is fundamental for guiding prevention and disease management strategies, ensuring better care and quality of life for patients and their families.
Anatomy, histology and physiology of the brain
The anatomy, histology and physiology of the brain are fundamental to understanding dementia in Alzheimer's disease.
The human brain is divided into areas that connect and perform complex and relatively specific functions, such as memory, language and movement. The outer layer, the cerebral cortex, is essential for complex cognitive processes. Nerve cells, or neurons, transmit electrochemical signals through connections called synapses.
Communication between neurons is mediated by neurotransmitters, which play a fundamental role in the transmission of information.
In the context of Alzheimer's disease, pathological changes affect these structures and processes. The accumulation of beta-amyloid protein plaques and the formation of neurofibrillary tangles interfere with the normal function of neurons, leading to degeneration and cell death.
In addition to the cerebral cortex, regions such as the hippocampus, which is crucial for the formation of new memories, are especially vulnerable to Alzheimer's disease. A detailed understanding of the anatomy, histology and physiology of the brain not only helps in understanding the symptoms of the disease, but also guides research into new therapies and preventative strategies.
Knowledge of this anatomopathological and histophysiopathological basis is essential for the application and development of effective diagnostic and treatment approaches aimed at mitigating the devastating impact of Alzheimer's disease on brain function and patients' quality of life.
Risk factors for Alzheimer's dementia
The risk factors for Alzheimer's dementia encompass a variety of genetic and environmental influences. Older age is the main factor, as the risk of developing the disease increases significantly after the age of 65. Family history also plays an important role, with studies suggesting that certain genetic variants may increase predisposition - for example the ApoE ε4 gene.
Lifestyle plays an important role; for example, a diet rich in antioxidants and omega-3 fatty acids can help protect against Alzheimer's dementia. In addition, regular physical activity and mental stimulation are associated with a lower risk.
Health conditions such as high blood pressure, diabetes and obesity can also increase vulnerability to Alzheimer's dementia, suggesting a link between cardiovascular health and brain health.
Environmental factors such as exposure to heavy metals and toxins may play a role, with research underway.
Understanding these risk factors is crucial to guiding prevention strategies. Promoting healthy lifestyle habits, monitoring health conditions and managing risk factors can help reduce the incidence of Alzheimer's dementia and improve long-term brain health.
Early diagnosis
Early diagnosis is important in Alzheimer's disease because it allows for the immediate start of treatments that can slow down the progression of the disease and improve the patient's quality of life.
Neuropsychological tests, which assess cognitive abilities such as memory, language and reasoning, are fundamental for detecting subtle changes that may indicate a neurocognitive disorder associated with Alzheimer's disease in its early stages.
Detailed clinical assessments, including a full medical history and physical examinations, help to rule out other conditions that can cause similar symptoms.
New brain imaging techniques, such as positron emission tomography (PET) and functional magnetic resonance imaging (fMRI), are also being used to detect changes in the brain associated with Alzheimer's even before obvious symptoms appear.
More recently, new test options with greater sensitivity and specificity have been incorporated to provide a more accurate diagnosis of Alzheimer's disease:
- Brain PET-CT with beta-amyloid marker: This uses brain images to identify deposits of beta-amyloid protein in the brain, which are indicative of the disease.
- Cerebrospinal fluid (CSF): Usually collected by lumbar puncture, CSF is analyzed to detect abnormal levels of beta-amyloid and tau proteins.
- Blood test (tau-phosphorylated 217, beta-amyloid ratio 42/40, APS2): Evaluates specific biomarkers in the blood that help identify the presence of Alzheimer's disease.
Pathology of Alzheimer's disease

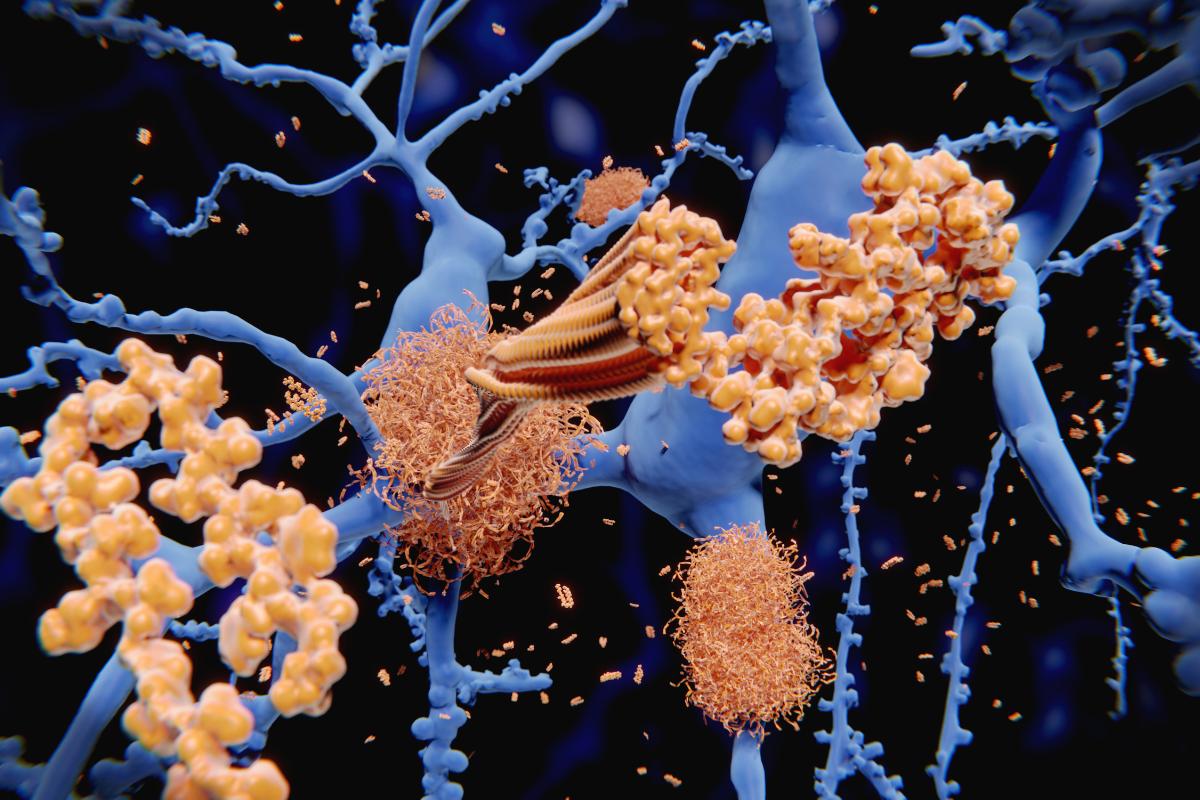
The pathology of Alzheimer's disease involves complex changes in the brain that directly affect cognitive function. The main characteristic is the accumulation of beta-amyloid protein plaques between neurons. These plaques interfere with neuronal communication and contribute to cell death.
In addition to plaques, neurofibrillary tangles also form inside neurons. These tangles are made up of a protein called tau - which loses its normal structure - and group together abnormally, causing additional cell dysfunction.
These pathological changes result in the progressive loss of neuronal connections and the degeneration of the neurons themselves, especially in areas of the brain responsible for memory and other cognitive functions. Chronic neuroinflammation is also observed in the brains of patients with Alzheimer's dementia, contributing to the cycle of cell damage and neurodegeneration.
A detailed understanding of these processes is crucial for the development of effective treatments that can interfere with the progression of the disease.
Current research is focused on therapies that can reduce the formation of beta-amyloid plaques and neurofibrillary tangles, as well as approaches aimed at neuronal protection and reducing brain inflammation.
This insight into the neuropathology of Alzheimer's disease helps to elucidate the biological mechanisms underlying dementia and to guide ongoing efforts to find therapeutic strategies that can improve the quality of life of affected patients.
Early symptoms of Alzheimer's dementia
The initial symptoms of Alzheimer's dementia can be subtle and easily attributed to normal ageing. Loss of recent memory is often one of the first manifestations, such as forgetting recent events or repeating questions. Difficulties in planning or solving simple problems can also appear, as well as impairment in the ability to perform usual tasks.
As the disease progresses, the symptoms become more evident. Disorientation about time and place is common, as are difficulties in understanding visual images and relating objects. Language problems, such as substituting terms incorrectly or difficulty finding the right words, are other indications.
In addition to cognitive symptoms, mood and personality changes can occur, including apathy, irritability and anxiety. As dementia progresses, the ability to carry out daily activities can be significantly compromised.
It is essential to recognize the early signs in order to seek specialist medical assessment. Early diagnosis allows appropriate interventions to be initiated, such as pharmacological and non-pharmacological therapies, which can help slow down the progression of symptoms and improve the quality of life of the patient and their carers.
Awareness of the early symptoms of neurocognitive disorder associated with Alzheimer's disease not only promotes more appropriate intervention, but also highlights the importance of preventative care and ongoing research to better understand and treat this complex neurodegenerative disease.
Variations in symptoms
The initial symptoms of Alzheimer's disease can vary widely from person to person, but two additional important aspects to consider are:
- Orientation problems: Individuals may begin to experience difficulties in orienting themselves in time and space. This can manifest itself through confusion about dates, seasons or even where they are located at specific times.
- Impaired decision-making: Another early symptom includes difficulties in making simple everyday decisions. This can be seen in situations such as choosing appropriate clothing for the weather or deciding what to eat at a meal, showing a gradual decline in the ability to carry out everyday tasks independently.
Recognizing these additional signs can help in the early identification of Alzheimer's disease, facilitating interventions that can help slow down its progression and improve the patient's quality of life.
Progression of symptoms
The progression of Alzheimer's dementia symptoms varies from person to person, but follows a general pattern of gradual deterioration of cognitive and behavioral functions.
Initially, mild symptoms such as occasional forgetfulness and difficulty finding words may appear. Over time, memory problems worsen, affecting the ability to recall recent events and recognize close people.
As the disease progresses to more advanced stages, other cognitive abilities are affected. Language can deteriorate significantly, leading to difficulties in verbal communication. In addition, motor skills can be compromised, making it difficult to perform simple everyday tasks.
Behavioral symptoms also intensify over time. Patients may experience more frequent and unpredictable mood swings, such as irritability, agitation or apathy.
As dementia progresses, it is common to see more pronounced spatial and temporal disorientation, as well as an increasing need for assistance with basic activities such as eating and personal hygiene.
Understanding the gradual progression of Alzheimer's dementia is key to planning appropriate care and support over time. This includes making adjustments to daily routines, implementing strategies to maintain patient safety and ensuring that their medical and emotional needs are met in a compassionate and effective manner.
Stages of progression
Alzheimer's dementia typically progresses through three main stages: early, intermediate and advanced. Each stage presents specific symptoms that progressively affect the patient's cognitive, functional and behavioral capacity.
Variations of Alzheimer's dementia
- Sporadic Alzheimer's dementia: This is the most common type of Alzheimer's dementia, representing up to 95% of cases. There is no clear genetic pattern and it is generally attributed to a combination of genetic and environmental factors.
The age of onset can vary, but usually occurs after the age of 65. Symptoms develop gradually over time, affecting memory, language and other cognitive functions.
- Familial or genetic Alzheimer's dementia: This type is less common, accounting for approximately 5% of cases. In general, it is inherited in a dominant way and tends to manifest itself at a younger age, around 30 to 60.
It is caused by specific genetic mutations, such as in the APP, PSEN1 and PSEN2 genes. People with a positive family history have a higher risk of developing the disease compared to the general population.
- Early-onset Alzheimer's dementia: Also known as early onset Alzheimer's dementia or onset before the age of 65, this type affects younger people.
It is less common and may be associated with specific genetic variants that cause the disease at a younger age than late-onset Alzheimer's dementia.
- Late-onset Alzheimer's dementia: It is the most common type of Alzheimer's dementia and usually affects people over the age of 65. Older age is the main risk factor, and the development of the disease is often related to factors such as age, family history and general health conditions.
Understanding these different presentations of Alzheimer's dementia is crucial for accurate diagnoses and for guiding personalized treatment and care strategies for each patient.
Diagnosis of dementia associated with Alzheimer's disease

The diagnosis of neurocognitive disorder associated with Alzheimer's disease involves a comprehensive assessment based on observed symptoms and clinical tests. Initially, the doctor takes a detailed clinical history to understand the symptoms and their impact on the patient's daily life. Cognitive tests are applied to assess functions such as memory, language and thinking skills.
Imaging tests, such as computed tomography (CT) or magnetic resonance imaging (MRI) of the skull, help to exclude other possible causes of symptoms and assess structural changes in the brain. Biomarkers in the cerebrospinal fluid (CSF), in a blood test or PET-CT brain images with a beta-amyloid marker can be used to detect abnormalities associated with beta-amyloid plaques and neurofibrillary tangles.
Differential diagnosis is essential to distinguish Alzheimer's disease from other conditions that may present similar symptoms, such as depression or vitamin deficits. A multidisciplinary team, including neurologists, psychiatrists and neuropsychologists, often collaborates to obtain an accurate diagnosis.
An early diagnosis is fundamental to starting interventions that can help slow down the progression of the disease and improve the patient's quality of life. As such, it allows patients and their families to plan properly for the future and make the most of the resources available to them.
Understanding the diagnostic process of Alzheimer's disease is crucial to promoting a holistic and integrative approach to patient care, providing comprehensive and personalized support throughout the disease journey.
Current treatments for Alzheimer's dementia
- Medications for cognitive symptoms: Cholinesterase inhibitors such as donepezil, rivastigmine and galantamine are commonly prescribed to delay the progression of impairment of cognitive functions such as memory, language and thinking.
They work by increasing levels of acetylcholine, a neurotransmitter crucial for communication between neurons in the brain affected by Alzheimer's disease.
- Medications for behavioral symptoms: In cases where symptoms such as agitation, anxiety, irritability or aggression are prominent, antidepressants, antipsychotics or mood stabilizers can be used at the doctor's discretion.
These medications help regulate mood and reduce disruptive behavior, providing greater comfort for the patient and improving interaction with caregivers and family members.
- Non-pharmacological therapies: Behavioral therapies focus on maintaining the patient's functional abilities, promoting independence in daily activities.
Physiotherapy can help maintain mobility and prevent complications arising from immobility. Music therapy, on the other hand, uses music to stimulate areas of the brain related to memory and emotion, offering comfort and well-being to the patient.
- Lifestyle-based approaches: Cognitive stimulation through games, puzzles and activities that challenge the brain can help preserve cognitive functions and slow down decline, but research is still ongoing.
Regular social activities are also beneficial, as they promote social interactions that are important for emotional and mental well-being.
- Supportive care: In addition to direct treatment for the patient, it is essential to provide emotional support for caregivers and family members, who play a key role in the day-to-day management of the disease.
Support programs, such as support groups and education about Alzheimer's dementia, help to provide a more informed and supportive care environment.
FDA approval of monoclonal antibodies
The US Food and Drug Administration (FDA) recently granted approval for the infusion of the monoclonal antibodies lecanemab and donanemab for the treatment of Alzheimer's disease. This milestone represents new hope for patients with mild cognitive impairment or early stage dementia associated with Alzheimer's disease, the focus groups of the clinical trials.
Donanemab is administered as an intravenous infusion every four weeks. The recommended dosage is detailed in the prescribing information, with an initial regimen of 700 mg every 4 weeks for the first three doses, followed by 1400 mg every 4 weeks.
The FDA's approval of donanemab is based on evidence of efficacy and safety. In a double-blind, placebo-controlled study (Study 1, NCT04437511), 1736 patients were randomized to receive donanemab or placebo for up to 72 weeks.
Patients treated with donanemab demonstrated a statistically significant reduction in clinical decline on the Integrated Alzheimer's Disease Rating Scale (iADRS) compared to placebo at Week 76. In addition, improvements were observed in the ADAS-Cog13 cognitive subscale and the ADCS-iADL scale.
The safety of donanemab has been carefully evaluated. The manufacturer's information includes a warning for amyloid-related imaging abnormalities (ARIA), which can present as temporary edema (swelling) in the brain or small bleeding points. Patients homozygous for the ApoE ε4 gene have a higher incidence of ARIA, suggesting the need for genetic testing before starting treatment.
In addition, there is a risk of infusion-related reactions, such as flu-like symptoms, nausea, vomiting and changes in blood pressure. Hypersensitivity reactions, including anaphylaxis and angioedema, have also been reported. The most common side effects were ARIA and headache.
The FDA has awarded donanemab "Fast Track", "Priority Review" and "Breakthrough Therapy" designations, reflecting the urgency and promise of this innovative treatment in the fight against Alzheimer's disease.
Administration and dosage of donanemab
Donanemab is administered by intravenous infusion every four weeks, as detailed in the manufacturer's information to ensure its efficacy and safety.
Patients initially receive 700 mg in the first three doses, followed by 1400 mg every four weeks. This protocol was established on the basis of rigorous clinical studies that assessed patients' response and tolerance to the drug.
It is essential that patients strictly follow the recommended dosage schedule and carry out infusions under medical supervision in order to monitor possible adverse reactions and adjust treatment as necessary.
Care and management of the disease
Caring for someone with Alzheimer's dementia requires a holistic and integrative approach to ensure comfort and quality of life. This includes:
- Safe environment: Modifying the home can include installing handrails, grab bars in the bathroom and adequate lighting to reduce the risk of falls. Removing unnecessary or potentially confusing objects helps to keep the environment clear and organized.
- Structured routineEstablishing fixed times for meals, activities and rest helps to reduce the patient's anxiety by providing predictability. This can also include schedules for medication and leisure activities.
- Clear communication: Use simple, direct language, with short sentences and pauses to allow the patient to process information. Avoiding complex or ambiguous conversations helps to minimize frustration and confusion.
- Cognitive stimulation: Activities such as puzzles, memory games and reading can help maintain cognitive skills. Music and art are also effective ways of stimulating the brain and promoting emotional well-being.
- Proper nutrition: A balanced diet rich in fruit, vegetables, whole grains and lean proteins is essential. Encouraging regular hydration is also important for general health and cognitive function.
- Emotional support: Both patients and caregivers can benefit from support groups, where they share experiences and learn coping strategies. Education about the disease helps to reduce stigma and increase understanding of the challenges faced.
- Medical monitoring: Regular consultations with healthcare professionals allow for adjustments in treatment as necessary. Periodic assessments help to monitor the progression of the disease and adapt the care plan accordingly.
Implementing these practices not only improves the quality of life of the Alzheimer's dementia patient, but also supports caregivers by providing them with resources and strategies to face the daily challenges of the disease.
Social and economic impact of Alzheimer's dementia
The impact of Alzheimer's dementia on society covers several crucial areas:
O social impact The burden of the disease is profound, affecting not only patients but also their families. Caregivers face significant emotional and physical challenges, often resulting in social isolation and emotional stress. The progressive need for intense care can negatively impact family dynamics and the quality of life of everyone involved.
In terms of economicAlzheimer's dementia generates substantial costs. The direct costs of medical care and indirect costs, such as loss of productivity at work and the need for caregivers, represent a significant burden on health systems and individual economies. These costs tend to increase as the disease progresses and more specialized care is required.
Within educationalAwareness of Alzheimer's dementia is essential. Lack of understanding about the disease can lead to social stigma and hinder access to adequate resources. Educating the population about the symptoms, care and support available is crucial to improving the quality of life of patients and caregivers.
Investments in research are fundamental to advancing our understanding of Alzheimer's dementia and developing effective treatments. Scientific advances can not only slow down the progression of the disease, but also improve the quality of life of those affected and reduce the costs associated with its management.
On one level politicalPublic policies aimed at supporting caregivers, promoting access to health services and encouraging research are indispensable. The implementation of policies that recognize and respond to the needs of people with Alzheimer's dementia and their families is important to mitigate the impact of the disease on society.
Psychological and emotional support

Psychological and emotional support plays a crucial role in the journey of patients and family members facing Alzheimer's dementia:
It is essential to provide a safe space for patients and their families to express complex emotions such as sadness, frustration and anxiety. This not only relieves emotional stress, but also strengthens general well-being.
Support groups play a valuable role as they offer a community of individuals who share similar experiences. These groups allow people in similar situations to connect, share information and offer mutual support, providing a sense of companionship and understanding.
Individual psychotherapy is an essential tool that offers not only a safe space to explore emotions, but also practical strategies for dealing with the emotional impact of the illness. Patients and caregivers can learn techniques to face specific challenges and develop effective coping skills.
Educating family members and caregivers about the behavioral and cognitive changes associated with Alzheimer's dementia is crucial. This not only improves understanding of the difficulties faced by the patient, but also equips caregivers with practical knowledge to deal with challenging situations in a more effective and empathetic way.
Offering caregivers ongoing support is essential to help them maintain a healthy balance between caring for themselves and caring for the patient. This can include access to guidance on personal care and monitoring caregivers' emotional well-being.
This comprehensive support not only benefits patients and caregivers directly, but also contributes to a better and more sustainable quality of life throughout the course of the disease.
Research and future developments
Alzheimer's research is at the forefront of current medicine, focusing on several key areas that could revolutionize the treatment and management of the disease.
New drugs are being rigorously studied to modify the progression of Alzheimer's disease, with the aim of destroying abnormal proteins and preventing the progression of beta-amyloid plaques in the affected brain.
Significant advances in imaging technologies, such as PET and functional magnetic resonance imaging, are making it possible to visualize structural and functional changes in the brains of Alzheimer's patients in greater detail. These technologies are essential for supporting early diagnosis and monitoring the progression of the disease.
New research has shown that more sensitive and specific diagnostic tests, such as brain PET-CT with beta-amyloid marker and biomarkers in cerebrospinal fluid (CSF) or blood, can provide greater accuracy in diagnosing the disease.
Genetic studies continue to identify genetic variants that increase the risk of developing Alzheimer's disease, allowing for personalized intervention strategies and the early identification of individuals most at risk.
In addition to the pharmacological treatments under development, research is exploring non-pharmaceutical interventions such as healthy eating, supplements, physical exercise and cognitive stimulation programs. These approaches have shown potential for slowing cognitive decline and improving patients' quality of life.
Global funding for Alzheimer's research is on the rise, encouraging multidisciplinary collaborations between academics, the pharmaceutical industry and non-profit organizations. This cooperation is essential for accelerating discoveries and translating basic research into significant clinical advances.
The future of research promises more effective and personalized therapies, more accurate diagnostics and more robust prevention strategies. These advances not only have the potential to improve patients' quality of life, but also to ease the burden on caregivers and healthcare systems, offering significant hope for those affected by this devastating disease.
Advances in the treatment of dementia in Alzheimer's disease with Dr. Petrus Raulino

Understanding dementia in Alzheimer's disease is not only essential for those facing the disease, but for society as a whole. This neurodegenerative condition not only profoundly impacts affected individuals and their families, but also represents a significant challenge for health systems around the world.
Throughout this blog, we have explored everything from the definition and history of dementia in Alzheimer's disease to the latest advances in research and treatment.
It is important to recognize the importance of early diagnosis and proper follow-up, as well as exploring the various therapeutic options available, both pharmacological and non-pharmacological.
Ongoing research and the development of new therapies offer hope for the future, promoting a better quality of life for patients and their families.
For those looking for effective, personalized treatment, make an appointment with Dr. Petrus Raulino could be the first step towards a better life.
As a doctor specializing in psychiatry, his evidence-based, patient-centered approach combines advanced knowledge of neurobiology with compassionate care, prioritizing not only emotional well-being, but also monitoring the organic biological factors that influence treatment.
Continue to find out about health conditions related to psychopharmacology at Dr. Petrus Raulino's blog and stay up to date on the best practices for dealing with dementia in Alzheimer's and other neuropsychiatric diseases.